Fibromyalgia is a disease categorized by widespread musculoskeletal pain, fatigue and poor sleep of at least three months duration that is not characterized by any other systemic or rheumatic disorder. While fibromyalgia is often a disease of exclusion after other causes are ruled out (such as rheumatoid arthritis and lupus for example), a good detailed history and physical exam can lean strongly toward the diagnosis. Changes in the diagnostic criteria in the recent literature have resulted in more cases meeting the diagnostic criteria for this disorder.
It is estimated that about two percent of the population in the United States has fibromyalgia. It is significantly more common in women than men and may be diagnosed in both adults and children. Other terms given to the disease include fibrositis, chronic pain syndrome, muscular rheumatism and myofascial pain syndrome. While the exact cause of fibromyalgia cannot be pinpointed, it appears to involve disordered signal processing that involves the pain pathways. Suggested as possible causes are hypothalamic-pituitary-adrenal axis dysfunction, inflammation, small fiber nerve problems, and infections such as Epstein-Barr, Lyme disease and even viral hepatitis. Bottom line—it remains unknown.
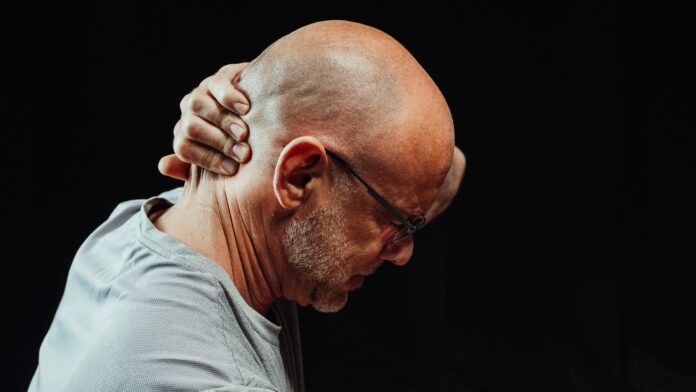
Pain is the most common symptom, involving muscles and ligaments and most common in neck, shoulder, back and hips. Diagnostic criteria historically involved multi-site pain from six or more of nine possible sites: Head, left arm, right arm, chest, abdomen, upper back and spine, lower spine, left leg and right leg. Sleep disorder, cognitive symptoms (such as poor concentration and forgetfulness), and diffuse tenderness in multiple areas are also accompaniments. The three-month period is used to exclude such causes as acute injury, viral infection, etc., owing to the chronic nature of fibromyalgia as a disorder.
The differential diagnosis of fibromyalgia is difficult because it shares symptoms with so many other diseases. In addition to the aforementioned rheumatoid arthritis and lupus, systemic sclerosis, polyarthralgia rheumatica, Lyme disease, hyperthyroidism, hypothyroidism and even early multiple sclerosis have to be considered and ruled out. Even medications such as statins in treatment for high cholesterol may cause symptoms similar to fibromyalgia. There are no specific blood tests or imaging that are specific for the disease, and as such it remains an exclusion diagnosis.
Treatment for fibromyalgia has been less than satisfactory. Patient education and self-management, exercise, cognitive behavioral therapy and hot and cold application have been used with only varying degrees of success. Studies with cannabinoids and marijuana use are early and have shown some benefit. Analgesics are given but not as primary therapy, as addiction to chronic pain medication is a worry. Antidepressant drugs such as amitriptyline (Elavil), pregabalin (Lyrica) and duloxetine (Cymbalta) also have been used, but often the side effects cause just as many problems as the disease itself. No universal treatment regimen to this point has proved satisfactory.
Fibromyalgia is generally not a concern in life underwriting for mortality, excepting that chronic pain may cause significant emotional distress and consequences. Associated depression, suicide, accidents, excessive use of alcohol or drugs, and adverse drug effects from treatment certainly affect prognosis. It is more the effects of chronic pain and disability (including absences and time off of work) that comprise the risk more the disease itself. Those must be considered in waiver of premium and disability riders and applications.
Perhaps the one limitation with fibromyalgia is in consideration for preferred status. Preferred consideration may be given when pain is mild, there are no physical limitations, low dose medication is used, there is no change in medication dosage and no continuous opioid or benzodiazepine use (which carry their own risks). Likewise there should be no concerns regarding alcohol or drug misuse and no associated psychiatric or concurrent medical diagnosis that increases risk on their own.